BLOOD CLOTS: Some are Good, Some are Bad!

The human body is an amazing organism. The amazing brain allows us to think, reason, and remember; the amazing heart pumps blood that supplies the body with nutrients and oxygen that keep it alive; and the other amazing organs carry out the many functions necessary to maintain the physical balance between normal and abnormal.
Central to all of this, and essential to the normal functioning of the body, and sustaining life is blood. This “life-giving” substance composed of liquid, called serum, and solid particles—red blood cells, white blood cells, and platelets—flows through blood vessels—arteries and veins—to every part of the body. Without blood life cannot continue. Each human body has a certain volume of blood that contains fixed percentages of white and red blood cells and varying numbers of platelets. Each component has a separate, specific function.
SERUM is the liquid part of blood. It is made up mostly of protein—albumin and globulin, fibrinogen and clotting substances called factors.
RED BLOOD CELLS transport oxygen and nutrients to the tissues. Too few RBC’s causes anemia and too many RBC’s (polycythemia) clog the vessels and affect organ function.
WHITE BLOOD CELLS are the body’s response to infection and stress. There are five major types of WBC’s which increase in number in response to the type of infection that is present.
PLATELETS are the cells which initiate the formation of blood clots. Too many platelets can cause the blood to clot too easily and a lack of platelets can cause bleeding.
BLOOD CLOTS are essential for the prevention of serious bleeding. But as with many things, there are GOOD blood clots and there are BAD blood clots.
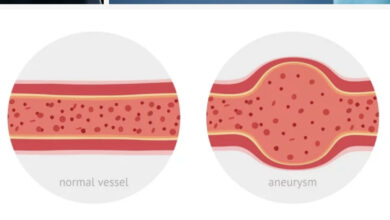
A blood clot that is in a fixed position is called a THROMBUS (Plural Thrombi).
A blood clot that moves in the bloodstream is called an EMBOLUS (Plural Emboli).
The process of clot formation is called THROMBOSIS.
The term for the movement of an Embolus is EMBOLISM.
The overwhelming majority of blood clots are the good type. Without the blood’s ability to clot, bleeding would continue until something is done to stop it. The loss of blood can lead to anemia, and the risk of bleeding to death from a wound is a significant concern. Hemophiliacs live with this situation every day.
Good blood clots form in response to an injury to the body. When the skin is lacerated (cut) blood vessels are also cut exposing the open ends which begin bleeding immediately. To begin the clotting process, the injured blood vessel constricts and contracts to try to shut off leaking blood. Circulating platelets accumulate at the site of injury and create a platelet plug. Then “clotting factors” circulating in the serum activate a series of chemical reactions (the Coagulation Cascade) and quickly a Fibrin and Red Blood Cell Clot forms. Active bleeding then stops. This is the normal process that protects humans from bleeding to death. This is a good thing.
A bad thing happens, though, when a clot forms within an intact blood vessel. These are Bad blood clots which can do two things:
1. Stay in the same, fixed location, enlarge, and eventually block the flow of blood in the
vessel.
OR
2. Break loose and flow through the blood stream until it reaches a vessel too small for it to
pass. It then blocks blood flow to the organ where it lodges. This “end organ” is most
commonly either the Brain or Lungs.
There are a number situations and factors that figure in to causing bad blood clots. They are:
1. Prolonged Inactivity: bed rest, traveling on long trips without getting up and walking
around, sitting at your desk with knees bent for long periods.
2. Surgery: especially hip and knee surgery, surgery for cancer (cancer patient’s blood is
hyper-coagulable—clots too easily).
3. Being in the hospital: 2/3 of all cases of blood clots in the legs occur while hospitalized.
4. Pregnancy: a hyper-coagulable state
5. Lifestyle habits: obesity, smoking, older age, sedentary activity.
6. Family history of blood clots
7. Major trauma: leads to inactivity
8. Drugs: estrogen-containing oral contraceptives, hormone replacement therapy.
9. Genetic disorders: Factor V Leiden
10. Certain types of cancer: pancreatic, lung, multiple myeloma, blood-related cancers.
11. Certain infections: HIV/AIDS, Hepatitis C, Lyme disease.
12. Autoimmune diseases
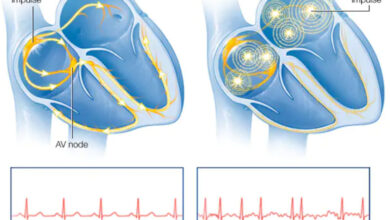
13. Arteriosclerosis: heart attack, arrhythmias (A-Fib), high BP, high cholesterol, PAD
14. Polycythemia Vera: the blood has an excessive number of RBC’s
15. Diabetes: everything diabetics have is worse
Anything that contributes to diminished blood flow within blood vessels can cause a clot. In most cases, more than one of the above factors are involved. So the best treatment, as I’ve said many times before, is prevention. Measures to limit immobility, increase movement, and being proactive are essential.
Most Thrombi form in the legs. Clots that form in the larger, deep veins are the ones of major concern. They are larger and more prone to embolize (break off and flow the lungs or brain). “Blood clots in the legs are responsible for hundreds of thousands of deaths worldwide…”
The terms for blood clots in the legs are:
Superficial Thrombophlebitis—a blood clot in a small surface vein. Thrombophlebitis
means inflamed (-itis), clotted (Thrombo), vein (phleb).
AND
Deep Vein Thrombophlebitis (DVT)—a deep vein is inflamed by a clot.
Symptoms of both differ.
Superficial—a small area of involvement is red, mildly swollen, and is warm and tender.
Deep—the affected extremity is swollen, painful, and very tender. It may or may not be red.
** Any patient with a single painful, swollen leg, has DVT until proven otherwise especially if they also have any of the factors listed above**
Most blood clots that Embolize lodge in the lungs. The term for this is Pulmonary (Lung) Embolus, Emboli (plural), or Embolism. They are used interchangeably. PE Blood Clots, as TV ads call them, are potentially fatal. Nearly 25% of cases do result in sudden death. They probably occur more often than is detected. PE clots end up in the smallest vessel they can’t pass through, cut off blood flow to that section of the lung, and that lung section dies (infarcts). Often multiple clot fragments embolize to the lungs and Infarct several sections of the lungs. The more clots in the lungs, the more lung damage, and the greater the likelihood of death.
Symptoms of blood clots in the lung are alarming and serious. Sudden Shortness of breath, chest pain especially with deep breathing, rapid breathing and heart rate, lightheadedness or passing out, and coughing up blood (if lung infarction has occurred).
Other embolizing blood clots go to the brain where blood flow is blocked to a section of the brain causing stroke symptoms. Blood clots to the brain more often form in the upper chambers of the heart (the atria) during an episode of Atrial Fibrillation.
That’s why Prevention is critical. Taking serious precautions during and after hospitalization and during and after major surgery is very important and anti-coagulating patients with A-Fib.
DVT is most frequently diagnosed by doing a Venous Ultrasound of the suspected extremity. This is a painless, non-invasive test that is highly reliable. The sound waves detect blood flow through veins and can see where blood flow is being impeded by a clot.
Prior to the improvement in ultrasound technology, DVT was diagnosed by performing a Venogram. This test required the injection of dye (contrast material) into a vein in the top of the foot; a painful and not-so-easy task. As the dye flowed upward, X-rays of the extremity were taken to find a blockage. Venograms were reliable tests but much more complicated to perform than ultrasound.
Detecting pulmonary emboli involves more effort. First—if a PE is suspected, a d-dimer blood test is done. Elevated levels of this material indicate damage to the lungs. Second—if the d-dimer is abnormal a V/Q Lung scan is done. V/Q stands for ventilation perfusion. This a Nuclear Medicine Test. In the ventilation phase, the patient inhales radioactive particles then the lung is scanned for damaged section that aren’t getting air. The perfusion phase requires an intravenous injection of a radioisotope that flows through the lung veins. The Lungs are scanned again, this time looking for “perfusion defects”—places where blood flow is blocked. Correlating these two phases, the nuclear medicine doctor (radiologist) can diagnose PE blood clots quite accurately.
A preferred, quicker, and more reliable test is a CT Angiogram. Here, dye is injected into an arm vein. It then flows into the lung veins. Using a CT scanner, the lungs are scanned for evidence of blockage to blood flow and damaged sections. This procedure has far better results and accuracy.
Treatment is aimed at attempting to reduce pain and inflammation, preventing more clots from developing and keeping the existing one from getting worse, and furthering the natural process of clot resolution as much as possible. Blood thinners and anti-inflammatory drugs are used. Details of treatment will be omitted in favor of a better understanding of the basics of blood clots.
References: nobility.nlm.nih.gov/biochemistry/clotting-factors/stat-pearls.
https://www.ncbi.nlm.nin.gov/books/NBK507850/
https://www.labtestsonline.org.au/learning/test-index/coag-factors-table
https://familydoctor.org/condition/blood-clots/
World Thrombosis Day: Dangerous Blood Clots: Know The Facts