AN EPIDEMIC OF A DIFFERENT COLOR: Atrial Fibrillation

I have at least 8 or 10 personal friends who have had episodes of Atrial Fibrillation. My wife and I have had it off and on for years, too. It’s such a common problem that it seems like a modern-day epidemic of a different type. Instead of a typical epidemic resulting from the rapid spread of an infectious disease, this disorder is not contagious, but the frequency seems to be increasing. More and more patients are having it. In and of itself, Atrial Fibrillation is fairly benign and not fatal, but it can lead to serious complications which are.
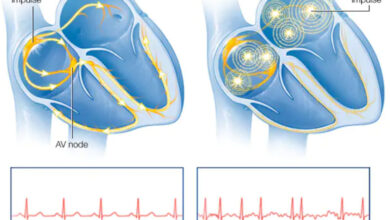
Atrial Fibrillation, or A-fib for short, is an abnormal rhythm of the heart. It’s a rapid, irregular, chaotic rhythm of the upper two chambers of the heart, the Atria. Heart beats normally originate from a specialized cluster of cells in the upper chambers (the Atria). This area is called the Sinus Node. It rhythmically and regularly emits electrical impulses that first spread over the Atria causing them to contract, then spread to the two lower chambers, the Ventricles, causing them to contract. This results in a steady, regular heart beat.
For a variety of reasons, impulses are sometimes emitted from other sites in the atria. However, these do not occur in a regular pattern but chaotically. Some of these impulses transmit to the ventricles and some do not creating an irregular rhythm and very irregular heart beat. Observers have described the heart in atrial fibrillation as resembling a wiggling bag of worms, while a normal heart beat looks like a hand repeatedly forming a fist.
In A-fib, the heart rate can be fast, very fast, or slow, but it is always irregularly irregular. Some patients have noticeable symptoms, some do not. A-fib comes in four types and may be:
Occasional (Paroxysmal)—it comes and goes lasting minutes to a few days, but it always stops on its own.
Persistent—episodes of A-fib last more than a week and often need medications or an electric shock (Cardioversion) to return to a normal rhythm.
Long-standing Persistent—episodes last longer than a year without going away.
Permanent—a normal rhythm cannot be restored. A-fib never goes away.
Causes of Atrial Fibrillation: The most common cause of A-fib is a structural abnormality of the heart.
Examples are disorders or abnormalities such as the following:
Abnormal heart valves—especially the Mitral Valve*
Heart Defects you were Born With (Congenital Heart Disease)
Heart Attacks (Infarction/Damage to Heart Muscle)
Coronary Artery Disease
Previous Heart Surgery
Conduction Disorders of the Heart (Wolff-Parkinson-White Syndrome)
Sick Sinus Syndrome—Malfunction of the Sinus Node
* The Mitral valve connects the upper and lower chambers on the left side of the heart.
The second most common cause is High Blood Pressure.
Next comes Lung Disease.
Pneumonia
COPD
Sleep Apnea
Pulmonary Embolism (Blood Clots)
Numerous other causes come next:
Chronic Kidney Disease
Overactive Thyroid State
Viral Infections
Diabetes
Alcohol, Tobacco, Caffeine—Stimulants
Illegal Drugs—Cocaine
Endurance Sports
Obesity
Stress
A large number of people have NO DISCERNIBLE CAUSE for A-fib and have what’s called Lone Atrial Fibrillation. This variety is usually intermittent (paroxysmal) and rarely causes serious complications.
An amazingly large number of patients, however, have A-fib and are completely unaware of it. They are asymptomatic. Their A-fib is found accidentally during a routine exam or when their BP or pulse is checked.
Patients who are symptomatic complain of heart palpitations, a fast irregular heart beat, weakness, shortness of breath, decreased exercise tolerance, mild vague chest pain, fatigue, lightheadedness or dizziness, or confusion, or they have an odd feeling in their chest.
The big concern in patients with A-fib is the major complications which can occur. These are:
Stroke
Blood Clots
Heart Attack
Heart Failure
Vascular Dementia
Sudden Cardiac Arrest—Rare
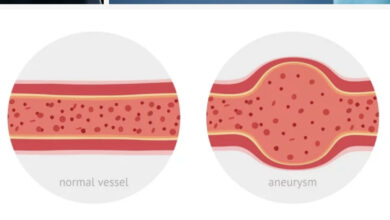
Stroke/Blood Clots—A-fib’s chaotic rhythm causes blood to pool within the heart’s upper chambers and form clots. Pieces of these clots break off and flow to the brain, blocking blood flow and causing a stroke. The clot fragment is called an Embolus. Doctors prescribe blood thinners for A-fib patients to prevent this complication.
Heart Attack/Failure—A-fib, if not controlled, weakens the heart leading to heart failure which means the heart pumps blood inefficiently. A-fib also increases the risk of heart attack in women in the first year after it’s diagnosed.
Vascular Dementia—A-fib increases the risk of Alzheimer’s disease due to blockages of blood vessels in the brain from loose fragments of blood clots.
Sudden Cardiac Arrest—A-fib increases the risk of the heart suddenly and unexpectedly stopping. The likelihood of this complication increases if the patient also has another serious heart condition.
When a patient has new onset Atrial Fibrillation they should have the following tests:
EKG—reveals the heart rhythm, size, and electrical axis.
Echocardiogram—Heart ultrasound to assess heart function, heart valves, and detect
structural abnormalities.
Blood Tests—for thyroid function, potassium, blood sugar, kidney function, anemia.
Chest X-ray—looks at lungs, determines heart size.
Sleep Study—to detect sleep disorders
Holter Monitor—if A-fib is suspected and the EKG does not show it, a Holter monitor
records heart activity for 24 hours or longer.
Exercise Stress Test—possibly.
TEE (Transesophageal Echocardiography)—special ultrasound of the heart to find blood
clots in the atria. The patient is sedated. An ultrasound probe is passed down the
esophagus to a location just behind the atria where clots form. An ultrasound is then
done to look for blood clots.
Treatment of A-Fib is a complicated subject in and of itself and will be covered in a separate blog at a later date.
Dr. G’s Opinion: Not a week goes by that I don’t hear that “so-and-so” has Atrial Fibrillation. It has become an incredibly frequent disorder among people in their 60’s, 70’s, and 80’s. Now that people aren’t smoking, we’re seeing a lot less coronary disease, sudden death, and heart failure. But instead, people are living longer and experiencing a significant increase in the frequency of arrhythmias like A-fib. The addition of blood thinners in the treatment of A-fib has reduced the frequency of the major complication of A-fib, Stroke, and new anti-arrhythmic drugs and radio frequency ablation procedures have improved quality of life for A-fib sufferers.
References: https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation