BABY, IT’S HOT OUTSIDE: How Heat Affects Our Bodies

Summer is coming! Here, in Arizona, it’s already arrived—today, the thermometer hit 95°. Summer officially starts June 21st, but in some parts of the country, especially the southwest, it’s already hot enough to begin to worry about the effects of heat on the human body. The average high temperature in Phoenix in April is 86°, in May it is 95°, June 105°, July 106°, August 105°, September 101°, and in October it is 90°. The average low temperature in July is 84°. So for seven months of the year, air temperatures are high enough for us to be concerned about heat-related illnesses. When the heat index is over 95°F, death rates increase, and the elevation of the temperature coupled with the duration of the heat bring about illnesses that range in seriousness from minor heat rash to near-fatal heat stroke.
People at risk are the elderly, the homeless, children, persons with heart and lung diseases, the physically disabled, patients with dementia, the obese, persons with poor fitness level, and persons who perform strenuous work outside. Medications may contribute to heat-related illness as well. Alcohol, diuretics, tranquilizers, antihistamines, beta blockers, calcium channel blockers, laxatives, anti-psychotics, and anti-depressants are just some of the drugs that affect hydration and body chemistry and are implicated in heat-related illness.
From 1999-2010, CDC statistics show there were 7415 deaths in the U.S. from heat-related illness. In the summer of 1980 alone, 1700 people died from heat exposure, and in the summer of 2003, “tens of thousands died in Europe.”
Statistics from the Arizona Department of Health Services show a need for awareness and prevention. From 2000-2016, in Arizona, there were 1193 heat-related deaths, 83% of these being in June, July, and August. Breaking it down demographically, 47% were AZ residents, 35% Mexican and Central American migrants, and 18% were from other U.S. states and Canada. The predominant age was 20-44 years for migrants and visitors while most AZ residents were over 45 years old. Of the total, 70% were males.
Median age at death for AZ residents was 59, those from other states and Canada 42, and migrants 29. During June, July, and August, Emergency Room visits and hospitalizations for heat-related illness are 7 times more common than for any other month. An ASU professor of Geographical Science and Urban Planning stated that “one third of AZ residents will have some kind of adverse health event in the summer months.” Notorious for heat-related disasters are the ill-prepared Grand Canyon summer visitors who make foolish, over strenuous hikes in temperatures over 100° F. They forget or are unaware that the south rim is 7000’ in altitude, and as they hike down into the canyon, the temperature rises significantly. At the Phantom Ranch, on the canyon floor, the temperature can be 30°-40° higher than at the rim. That’s a set up for real trouble if visitors don’t prepare adequately.
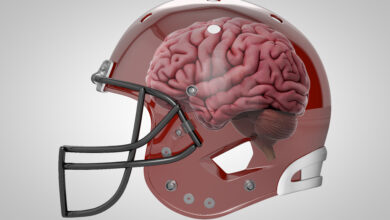
What happens to the human body when it becomes overheated? The body’s temperature control is regulated by the brain (hypothalamus) and the spinal cord. Normal body temp is 98.6°F. When exposed to heat, temperature sensors in the skin cause dilation of blood vessels which leads to sweat production. Sweating is the body’s mechanism for releasing heat, and as sweat evaporates the body cools down. But as the heat persists and the patient becomes dehydrated through lack of water intake and continued sweating, trouble begins.
To protect the “core” of the body, the previously dilated blood vessels constrict (narrow down) redirecting blood to the organs to protect them. As this occurs, several acute physiologic alterations occur that raise the body’s core temperature. When a person’s core temperature reaches 104°F, cellular damage occurs, there is an inflammatory response system-wide, endotoxins (harmful proteins) are released, and organ dysfunction occurs. Then symptoms develop.
There are five Heat-Related Illnesses. In order of severity they are:
Heat Rash
Sunburn
Heat Cramps
Heat Exhaustion
Heat Stroke
Each of these disorders is significant, but heat exhaustion and heat stroke can have serious consequences and even fatal outcomes.
Heat Rash: is clusters of small, red blisters resembling pimples, found on the neck, chest, groin, and elbow creases caused by sweating during hot, humid weather.
Treatment: Move to a cool, dry place, keep rash dry, apply baby powder for comfort
Sunburn: first degree (redness) and second degree (blistering), painful burn damage to the skin from ultraviolet light overexposure.
Treatment: avoid further sun exposure, apply cool cloths, cool baths, apply moisturizing lotion
Heat Cramps: muscle spasms in the abdomen, arms, legs, during strenuous exercise and heavy sweating. The loss of salt (sodium), electrolytes, and water cause cramps
Treatment: stop physical activity, drink water or electrolyte sports drink, move to a cool place
Heat Exhaustion: symptoms are heavy sweating, cold clammy pale skin, rapid pulse, nausea, vomiting, dizziness, cramps, headache, weakness, fainting occurring after prolonged heat exposure and inadequate replacement of fluids and electrolytes.
Treatment: move to a cool place, loosen clothing, drink cool beverages slowly, apply cool wet cloths to the skin. If vomiting, lethargic, or symptoms last longer than an hour, get medical help
Heat Stroke: a serious, life-threatening situation. Body temperature exceeds 103°F, skin is hot red, dry or damp, rapid pulse, headache, dizziness, nausea, confusion, loss of consciousness, coma, death.
Treatment: call 911 and get immediate medical help, move to cooler place, lower body temp with cool cloths or cool bath, spray with cold water, fan vigorously, don’t give oral fluids.
The adage “an ounce of prevention is worth a pound of cure” definitely fits this situation. The best treatment for heat-related illness is prevention. Following the recommendations below will keep you out of trouble and avoid potentially lethal consequences.
Prevention of Heat-Related Illness:
1. Avoid prolonged heat and sun exposure—take shade breaks, go inside to cool down
2. Drink adequate water, even if you’re not thirsty. Thirst is a late sign of dehydration.
3. Replace salt and minerals with sports drinks
4. Wear light-colored, loose-fitting clothing
5. Apply sunscreen every 2 hours or after swimming
6. Avoid caffeine drinks and alcohol
7. Never leave children or pets in a car
8. Enjoy outdoor activities in early morning or late evening hours
9. Wear a hat, keep babies out of direct sun
Dr. G’s Opinion: Heat-related illnesses are a significant problem in some parts of the country. Common sense, good judgement and decision-making, and not taking dangerous risks are the best way to initiate prevention. Always being well-hydrated and having access to adequate water and electrolyte replacement are essential tenets. Most people who end up in trouble don’t do the recommended preventive measures, or they make bad, reckless decisions. But if we were all perfect none of these disasters would occur. So avoid over exposure, drink fluids, and stay cool. We old folks need to be careful.
References: Gauer R, Myers BK, “Heat-Related Illnesses” American Family Physician 2019 Apr 15;99(8):482-489.
Becker JA, Stewart LK, “Heat-Related Illness” American Family Physician 2011 Jun1;83(11):1325-1330.
maricopa.gov/2457/signs-of-heat-illness
CDC.gov/heat-related-illness