HEMORRHOIDS

Four years ago, I wrote a blog on common anorectal problems. Among those, the most common was hemorrhoids. In one study, hemorrhoids had a prevalence of 39% meaning in one year’s time, just under half the population will have symptoms or findings of hemorrhoids. A lot of cases go unreported because the patient wasn’t bothered badly enough to see a doctor.
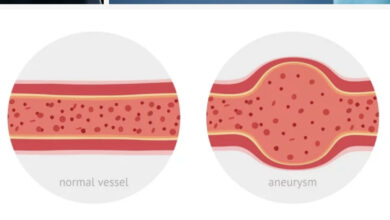
Hemorrhoids are somewhat like having varicose veins in the rectum. Because of increased intr-abdominal pressure from constipation, straining to defecate, or pregnancy, the anorectal area becomes engorged with blood causing the tissues to stretch, expand, and begin to protrude from the rectum. Eventually, the pressure from engorgement becomes enough to thin the surface of the rectum causing bright red blood to appear in the commode or on toilet tissue. The most common symptom of hemorrhoids is rectal bleeding and vice versa, the most common cause of rectal bleeding is hemorrhoids.
Hemorrhoids can be either internal (inside the anus and visible only by anoscope) or external (right at the anal opening). They occur in three places in the rectum where clusters of blood vessels are prominent. These places are left lateral (3), right anterior (11), and right posterior positions (7). With the patient in the lithotomy position) on his/her back with legs up in stirrups, the positions are at 3 o’clock, 7 o’clock, and 11 o’clock. The locations are designated by the patient’s right and left sides. The 7 o’clock position, which is right posterior, is the most frequent location.
In addition to bleeding, hemorrhoids cause pain, itching, swelling, and prolapse. Prolapse is the term used when the hemorrhoids protrude through the anal opening and are visible or palpable. Prolapse is also used in grading the severity of hemorrhoids. There are Grades I through IV, with IV being the worst. To better understand these designations, the following explanation is based on the anatomic abnormality and functional limitation.
GRADE I: Hemorrhoids bleed with defecation but do not prolapse—73% of cases
GRADE II: Hemorrhoids prolapse with defecation and retract spontaneously—18% of cases
GRADE III: Hemorrhoids prolapse and require manual retraction—8% of cases
GRADE IV: Hemorrhoids prolapse and can’t be retracted—1% of cases.
Many people with hemorrhoids have no symptoms. These patients don’t realize they have a problem until the condition gets bad enough to cause a symptom. Age also plays a role in patients with hemorrhoids because most patients with symptoms are over 50 and worsen as they get older. Some hemorrhoids are so engorged with blood they become thrombosed, ie. the blood in the hemorrhoid becomes clotted. Thrombosed hemorrhoids cause a persistent swollen lump in the rectum, are painful, and are prone to bleed. Occasionally, a clot will expand causing the surface of the hemorrhoid to thin out and leak blood or cause persistent pain.
The first pillar of treatment is a diet high in fiber. Avoiding foods that cause loose stools and irritate the rectum are important, too. First and second grade hemorrhoids are usually treated non-surgically with a topical cream, like cortisone, sitz baths in warm to hot water, or a soothing suppository which reduces swelling, pain, and itching. Grade III hemorrhoids are treated with rubber band ligation or a hemorrhoidectomy while Grade IV always require surgery. Rubber band ligation is an outpatient procedure in which a very small rubber band is placed at the base of the hemorrhoid cutting off the blood supply. Results are good and post-operative recovery is comfortable.
Hemorrhoidectomy, the accepted gold standard for treatment, is also outpatient, but recovery takes 2-3 weeks and is accompanied by considerable rectal discomfort. Sitz baths are helpful to a degree, but it’s only the passage of time that serves to make the post operative pain any better. Another effective procedure is hemorrhoidal artery ligation. Using a Doppler-equiped proctoscope, branches of the hemorrhoidal artery that supply blood to hemorrhoids are located and tied off (ligated). Interrupting the blood supply to the hemorrhoid causes the tissue to die and slough off. Hemorrhoidectomy is the preferred method of treatment, but hemorrhoidal artery ligation is gaining acceptance.
The prevalence of hemorrhoids is greatest in middle-aged males in the right posterior position. Rectal bleeding is the most common symptom, and treatment is relatively successful. Surgery can be avoided by maintaining a high fiber diet and using a cortisone or anti-inflammatory cream at the first sign of problems. Although, most patients don’t require surgery, it remains a useful option for patients with more severe problems.
References: von Roon AC, Reese GE, Tekkis PP. Hemorrhoids: hemorrhoidal artery ligation. Clinical Evidence 2014 Oct;01:415.
Ray-Offor E, Amari S. Hemorrhoidal Disease: Predilection Sites, Pattern of Presentation, and Treatment. Ann Afr Med 2019 Jan-Mar;18(1):12-16.
Guttenplan M. The Evaluation and office management of hemorrhoids for the gastroenterologist Current Gastroenterol Rep 2017 July;19(7):30
Pata F, Sgro A, Ferrara F, Vigorita V, Gallo G, Pellino G. Anatomy, Physiology, and Pathophysiology of Hemorrhoids. Rev Recent Clin Trials 2021;16(1):75-80.
Colin JF, et al, Hemorrhoids. A Review. Acts Gastroenterol Belg 1995 Sept-Dec;58(5-6):452-464.