SHORTNESS OF BREATH

Doctors call shortness of breath a single, much shorter name—Dyspnea. The Greek and Latin derivatives of dyspnea are “dys” which means bad or ill, and “pnea” which means breathing. So dyspnea is bad, or ill, breathing. Other such examples are “Apnea” meaning absence of breathing and “tachypnea,” rapid breathing. Dyspnea is much shorter to write and say and is used all the time in medical records. A patient who is short of breath is “dyspneic.” A person who gets short of breath with activity has “dyspnea on exertion.” If one suddenly awakens short of breath in the middle of the night, he/she has “paroxysmal nocturnal dyspnea.”
Dyspnea is a common symptom. Like chest pain, shortness of breath gets peoples’ attention, immediately. When you can’t get enough air it is very scary and people want that symptom addressed right away. Dyspnea occurs when the body’s demand for air (oxygen) exceeds the ability to obtain it. Something wrong with the body keeps the patient from getting the air he/she needs to be comfortable.
The causes of Dyspnea can be narrowed into three basic categories. They are:
Cardiovascular causes—a heart problem
Pulmonary causes—a lung problem
Metabolic causes—a chemical imbalance in the patient’s system
The elderly have the greatest likelihood of having multiple reasons to have dyspnea. Being overweight, out of shape, or anemic are common reasons for dyspnea in the elderly. Anxiety is a very common cause of dyspnea, or at least the sense of breathlessness like during a panic attack. Far more serious, though, are cardiac and pulmonary causes.
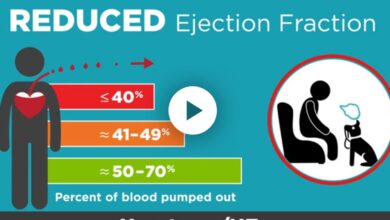
Cardiac causes range from coronary disease, to arrhythmias, to heart valve leakage or blockage problems, and to weakening of the heart muscle (cardiomyopathy). The lungs cause dyspnea because of infections (pneumonia, bronchitis, TB), asthma, COPD, tumor or cancer, aspiration and airway obstruction, inhalation or toxic chemicals or gasses, pulmonary fibrosis, pulmonary hypertension, pleurisy, and acute pulmonary emboli (blood clots in the lungs). Allergy problems are a common cause as well.
Metabolic causes can be a lot harder to diagnose. If the patient’s blood becomes acidotic, dyspnea occurs. When this type of dyspnea is present, there is usually no obvious, visible cause unless something abnormal shows up in the blood. For a number of reasons, carbon dioxide can build up in the blood stream causing the blood to become acid. Excess CO2 in the blood triggers a reflex dyspnea during which the patient exhales as much carbon dioxide as possible correcting the acidosis. Kidney failure, an overactive thyroid, septicemia, and fever are a few of other metabolic causes of dyspnea. Increased pressure on the brain, stroke, brain tumor/infection can cause dyspnea, too.
To determine the cause of dyspnea, in the past, doctors relied on blood drawn from an artery. Most blood tests are done on venous blood, but for dyspnea, arterial blood is required. The oxygen level in arterial blood is higher than in venous blood, while carbon dioxide levels are low—or should be. The pH of the blood (acid/base level) is determined as well. This was a time consuming, cumbersome method to obtain blood oxygen levels and has almost totally been replaced, today, by pulse oximetry. A pulse oximeter is the small clamp device placed on your finger. It gives an oxygen saturation reading immediately. A normal reading is 90% or higher. The clamp can be left in place for continuous monitoring of the oxygen level. When it is determined the oxygen level is low, multiple other diagnostic tests are done to determined the cause.
Using the patient’s history and physical exam, the doctor should get some information that points in the direction of the cause. Testing is done in an orderly fashion on a trial and error basis to determine the cause and treat it. A chest x-ray, EKG, chest CT, and breathing function tests are good baseline studies. For cardiac causes, an echocardiogram, and even a cardiac cath, are very helpful. Many of the diagnoses that cause dyspnea are bad things to have. But starting treatment that corrects the problem usually improves the symptoms.
Dr. G’s Opinion: As Kareem Abdul Jabbar said in the TV commercial, don’t ignore dyspnea. He did and experienced severe symptoms before he was diagnosed with atrial fibrillation. Dyspnea is a “cardinal symptom” of heart and/or lung disease and demands attention. Yes, you may be obese and out of shape, but you don’t know that until you’ve been fully evaluated. Until you’ve be checked for a serious heart or lung problem, you shouldn’t start exercising to shed those pounds.
References: Bozkurt B, Mann DL. Update: Shortness of Breath Circulation 2014 Oct;129(15):447-449.
Hauswaldt J, Blaschke J. Dyspnea Internist (Berl) 2017 Sep;58(9):925-936.
Mahler DA. Evaluation of Dyspnea in the Elderly. Clin Geriatr Med 2017 Nov;33(4):593-521.
Anzueto A, Miraviltlles M. Pathophysiology of dyspnea in COPD. Postgrad Med 2017 Apr;129(3):366-374.