BLOOD THINNERS AND ATRIAL FIBRILLATION: Who Should Take What?

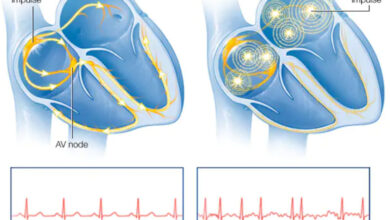
Since 2014, the American Heart Association, the American College of Cardiology, and the Heart Rhythm Society have recommended a set of guidelines for the treatment of the various forms of Atrial Fibrillation and Atrial Flutter. The biggest area of disagreement in these guidelines has been the decision to prescribe or not prescribe blood thinners (anti-coagulation) for stroke prevention. The U.S. Food and Drug Administration has recently presented new information that clarifies that confusing subject, and gives doctors reliable, specific criteria that make that decision easier.
So many factors are involved in the decision that I approach it cautiously so as not to bore you with details. BUT, taking blood thinners is not without risk and not taking blood thinners when you have chronic atrial fibrillation can lead to a debilitating or fatal stroke. So it’s no small matter.
These multiple risk factors have been consolidated into the acronym CHADS-VASC. Each letter stands for a condition or circumstance whose point values, when added together, determine who needs a blood thinner. Each criteria has one or two points. Women with at least 3 points and men with 2 or more points need blood thinners. What follows is a list of these criteria and their point values. If one has any of the listed conditions, the point values are totaled, and a decision reached.
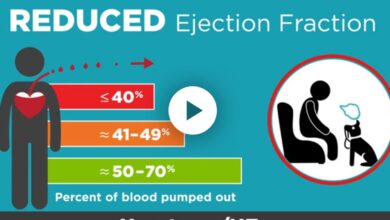
C = Congestive Heart Failure—1 pt
H = Hypertension—1pt
A = Age at least 75 years—2pts
D = Diabetes Mellitus—1pt
S = Previous Stroke, TIA, Blood Clot—2pts
V = Vascular Disease—1pt
A = Age 65-74–1pt
Sc = Sex—1 pt
Women only need 3 points and men only 2 to be prescribed oral blood thinners so the threshold for anticoagulation is quite low. Thus it is easy to see that most people in Atrial Fibrillation need anti-coagulation.
Drugs such as Pradaxa, Eliquis, Xarelto, and Savaysa are preferred over Coumadin (Warfarin) for safety and ease of dosing. However, if the patient also has moderate or severe mitral valve stenosis (narrowing) or has a mechanical (artificial) heart valve, warfarin is the preferred drug.
Dr. G’s Opinion: Many years ago, a friend of my parents, a woman in her 50’s, suddenly had a stroke. I later learned she had had rheumatic fever as a young woman and had chronic atrial fibrillation and mitral stenosis (a narrowing of blood flow through the heart valve between the 2 chambers of the left side of the heart). Her health was declining rapidly, and after having another stroke, she passed away.
During my early years of practice, a female patient of mine, in her 70’s, had a devastating stroke. She also suffered from chronic atrial fibrillation and mitral valve narrowing (stenosis). She had had these conditions for years, but treatments in the 60’s and 70’s were primitive by today’s standards. Neither of these women were on blood thinners, nor were doctors at that time aware of the benefits of anticoagulation for patients such as these.
Today’s practitioners would routinely prescribe blood thinners to these two women. They would still be at risk of having a stroke, but their chances would be far, far less. Brilliant and innovative researchers have discovered criteria, protocols, and treatments that give patients a better quality of life and protect them from the complications of atrial fibrillation. Anticoagulation is one of them.
Atrial fib, by itself, is not a fatal arrhythmia, but the problems it can cause and the complications associated with it certainly are. Anticoagulation has definitely been shown to protect the quality of life for A Fib patients and contribute to longevity. When your doctor recommends it do not be fearful, but be thankful he is doing what’s best for you.
References: Practice Guidelines. Management of Atrial Fibrillation: Updated Guidance from the AHA, ACC, HRS. Am Fam Phys 2020 Jan 15;101(2):123-124.