NEW CPR GUIDELINES FOR INFANTS, CHILDREN
Have you ever imagined what it would be like to do CPR (cardiopulmonary resuscitation) on an infant or small child? Thankfully, it’s something not often required, but think about doing external chest compression on a baby. Using both hands, you’d break every rib in the chest. Or if you did mouth-to-mouth breathing, you’re certain to blow out both lungs. It would be a disaster.
Newborn infants probably require CPR more than any pediatric age children, especially those born prematurely, or babies with extremely difficult deliveries. The hospital delivery room is a frequent site of resuscitation, even if it’s only vigorous toweling to clean off fluids from delivery. Tactile stimulation causes robust crying and squirming that gets those lungs breathing and the heart beating. But others require full CPR which must be modified to prevent unnecessary injury.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have recently announced significant changes in technique recommended for CPR in infants. The changes are significant for improving the safety and efficacy of CPR. Why is this important? Well, because I think it’s interesting, and it’s something you, the lay public, have never thought about or know very little.
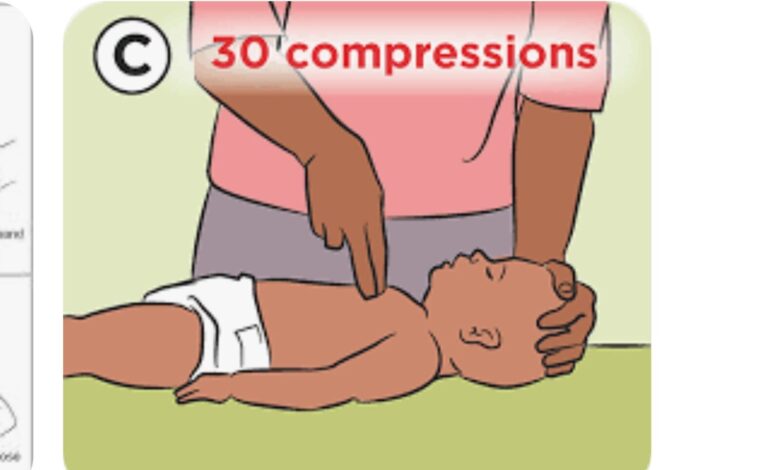
Chest Compression: Until recently, “two-finger chest compression” was the standard. The tips of the index and middle fingers were used to compress the chest and simulate the heart to beat. Instead, it is now recommended to wrap the “rescuer’s hands around the infant’s chest and the two thumbs [are] pressed down on the sternum (breastbone).” Why the change? “Studies have shown the two-finger chest compressions generate less force than using the two-thumb encircling technique.” It’s also easier to control the baby and feel how much force you’re exerting. Thirty chest compressions are recommended followed by two breaths into the airway. Then 30 more chest compressions followed by 2 breaths, then on and on.
Breathing Support: This can be done by either using mouth-to-mouth breathing or an infant Ambu bag, if available. An Ambu bag is a mask connected to an inflatable bag. The mask covers the patient’s nose and mouth and squeezing the bag forces air into the baby’s lungs. Ambu bag breathing is preferred because breathing force and volume are controlled and collapsing the lungs is less possible. The two breaths are done, one every 2-3 seconds after chest compressions.
Foreign Body Removal from the Airway: The Heimlich maneuver has been the standard of care for decades. The rescuer standing behind the victim, makes multiple forceful thrusts to the pit of the stomach with clenched fists until the obstructing object is forced or coughed out of the airway. Now, the AHA and AAP are recommending the “inclusion of blows to the back to clear foreign body airway obstruction in children….The guidelines recommend cycles of five back blows followed by five abdominal thrusts.”
Umbilical Cord Clamping: This is not a part of CPR technique, but the need for cardiorespiratory support is reduced by waiting “at least 60 seconds after birth” to clamp and cut the umbilical cord. This allows an extra “transfusion [of blood] from the placenta [and] is beneficial in both term and preterm infants.”
Dr. G’s Opinion: These are great improvements that provide safety and efficacy. Nothing is scarier than an infant who’s not breathing, so it is hoped these new techniques will improve outcomes.
Reference: www.medscape.com/new-CPR-guidelines-aim-to-save-more-young-lives/
Sandberg B. New CPR Guidelines aim to save more young lives. Medscape 2025 October 30.




