HOME INR TESTING FOR WARFARIN
Are you one of the 6 million Americans who have atrial fibrillation? If so, do you take a blood thinner (anticoagulant)? If you don’t, you should because folks with A Fib have a five times greater risk for stroke than folks who don’t have A Fib.
Anticoagulants come it two “generations.” The first, or older generation, of anticoagulant is warfarin known commercially as Coumadin. It is a slow-acting, long lasting drug that is affected by numerous foods and medications. The effect of warfarin on thinning the blood can be increased or decreased simply by what you eat or what drugs you take, and the dose you take can vary frequently.
The second “generation” of anticoagulants was introduced to the public between 2010 and 2013. The three drugs is this group are Pradaxa (dabigatran), Xarelto (rivaroxaban), and Eliquis (apixaban). These drugs plus warfarin are all orally administered. They all also have the risk of bleeding episodes especially during the first 3 months of use. Second “generation” blood thinners have fixed dosing, ie. one dose works for everyone.
(There also are injectable blood thinners which are indicated for rapid onset and short term anticoagulation. They are heparin, Lovenox (enoxaparin), and Arixtra (fondaparinux). These are not part of this discussion as they are not used long term in A Fib).
Between the two “generations” of oral anticoagulants there is a factor that separates them and helps many patients decide which generation is right for them. That is the need for frequent monitoring by blood tests. Patients on warfarin must have a PT/INR blood test at least monthly to monitor the “thinness” of the blood, while newer drugs require no such monitoring. The dose of warfarin is different for every patient, and the blood thinning effect on each person varies as well, completely depending on diet and medication. Patients on warfarin find that some foods thin the blood while others thicken it. Thus once a month, or more frequently, a blood test is necessary to monitor if one’s blood is at the ideal level of anticoagulation.
The test is called a PT/INR, or just INR. PT stands for Prothrombin Time, or Pro Time for short. INR stands for International Normalized Ratio. INR is the preferred test for accuracy and consistency. An INR can be done from a venous blood sample in the lab or at home, or anywhere, by a finger-stick.
Finally, I get to the real subject of this blog—Home INR Testing. In 2020, the Coumadin Clinic nurse who was following my monthly INR’s drawn at a local lab, suggested I try finger-stick home INR testing. She said it would save me going to the lab and being stuck twice in each arm, and finally, in the back of my hand, to find a vein that would yield a decent blood sample. After decades of venipunctures in the same veins, the veins get scarred and drawing a blood sample becomes difficult. So not dealing with that plus avoiding a trip to the lab were welcome benefits. I agreed to give home testing a try.
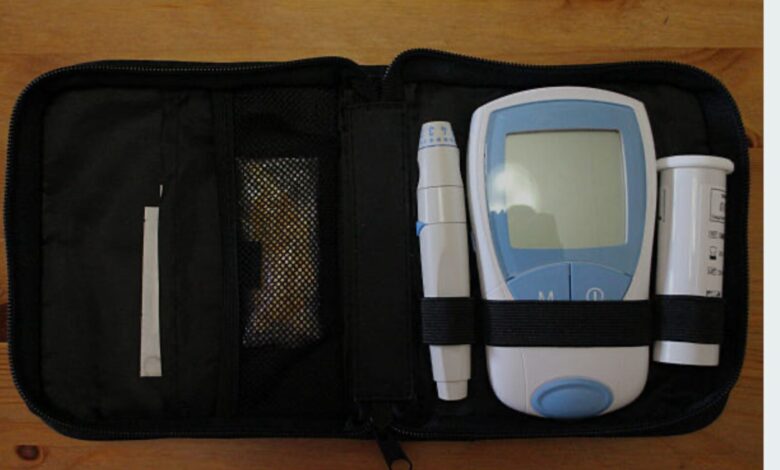
I received everything I needed in the mail. A case/kit containing test strips (10 per container), fingerstick lancets, a log book/pamphlet to record my results, and the monitor itself. Extra test strips and lancets were included. Medicare covered the entire cost. A company in California, Acelis Connected Health, was the provider of supplies, and the receiver of my results via an app on my iPad.
Learning the technique took awhile. I used at least four test strips and stuck myself as many times before I got it right. A test strip slides into a slot in the bottom end of the monitor turning it on. I then have 180 seconds (3 minutes) to stick my finger and place a drop of blood on the strip. The tricky part is getting a decent hanging drop of blood. If I succeed, the monitor beeps, and the INR result appears in 10 seconds or less. The monitor stores the results, and I also record them in my log book. I then enter my results into the app on my iPad, and they are sent to the Coumadin clinic.
If my drop of blood is too small or not placed on the strip just right, the monitor gives me an error message. If that happens, I start all over. Acelis keeps track of how many strips I use and sends more when my supply runs low. Lancets, too. This is all covered by Medicare and no cost to me.
Home INR monitoring is a huge time saver. It is easy (I can test in 5 minutes or less), and completely trouble-free. The Coumadin clinic calls to tell me my results (which I already know), or contacts me through their electronic medical record website. Any dosage changes are made through this communication. I test every two weeks, but if my INR is out of range, I am able to test more frequently if needed.
DrG’s Opinion: Home INR testing is something I highly recommend. It saves time, costs nothing, and is accurate. Knowing if your blood is too “thick,” or too “thin” is important for preventing a stroke or a serious hemorrhage. It is simple, easy, and quick. There are many reasons to do it, all of which are good. Give it a try.





Interesting.