BRAIN CHANGES SIGNAL SUBSTANCE ABUSE
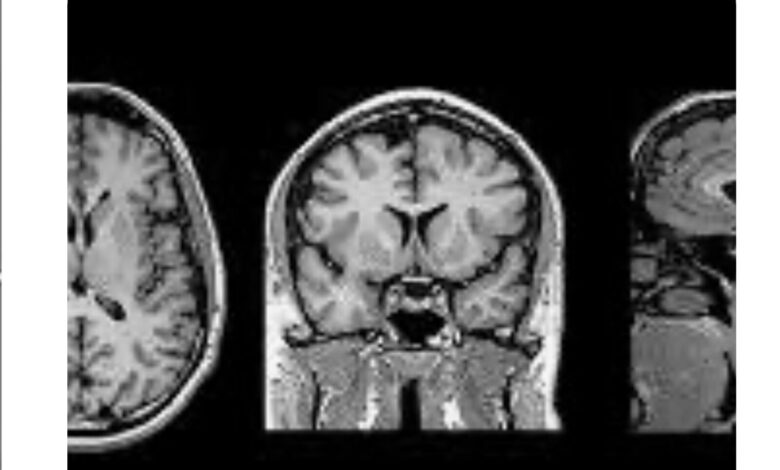
Brain changes seen in youth may signal future substance abuse problems: It has always been thought that substance abuse (alcohol, nicotine, cannabis, other illicit drugs) caused the brain changes (thinning of cortex, low volume of gray matter, less white matter stability) seen in youths (average age 9.9 years) who abuse these substances. But recent information learned from a study at the Indiana University School of Medicine says just the opposite. Children who show the above-noted neuroanatomical changes on imaging studies are at higher risk for substance use/abuse disorder than those who don’t. So the abnormalities of the brain actually are thought to be responsible for substance abuse rather being the result of it.
Nine thousand eight hundred and four children, average age 9.9 years had baseline brain MRI’s. Of this total, 3460 experienced substance abuse before age 15. They were followed yearly for 3 years. Compared to children who did not abuse substances, those who did all had neuroanatomical changes at baseline. Substance abusers had thinner cortex (surface layer) in the frontal lobe regions and larger brain volumes and deeper sulci (the spaces between brain sections). Analysis of 1203 youth who began substance abuse after the baseline MRI, found that most, if not all, had brain abnormalities that preceded substance abuse.
It seems, then, that the egg did indeed precede the chicken and thus brain changes associated with substance abuse problems are present at baseline. Much more needs to be learned, but this is an excellent start.
I know this information is probably more pertinent to physicians because of the technical complexity of the content. But it implies that some people are genetically “destined” to be substance abusers, rather than having a serious behavioral problem.
Reference: Anderson P. Brain Changes in Youth who use Substances: Cause or Effect? Medscape Medical News 2025 January 3.



